What is chronic obstructive pulmonary disease?
Chronic obstructive pulmonary disease, well known by the acronym COPD, is a disease characterized by obstruction of the airways. It encompasses two diseases, chronic obstructive bronchitis and emphysema. A person living with COPD can have both diseases or one of them.
The Quebec Lung Association defines chronic obstructive bronchitis as “a permanent inflammation of the bronchi often accompanied by hypersecretion of mucus which makes it difficult for air to pass to the lungs”. The inflammation and the build-up of mucus narrows the diameter of the bronchi and limits the amount of air that can circulate. Its main symptoms are shortness of breath, chronic cough and excessive secretion production. Emphysema, on the other hand, is a degenerative disease characterized by the destruction and loss of elasticity of lung tissue, more specifically the alveoli. When the alveoli are dilated and their walls damaged, the gas exchange that normally occurs in them is reduced, the air remains trapped and the amount of oxygen that can be delivered through the body is restricted. The main symptoms of this disease are shortness of breath and weight loss often accompanied by a cough (more common in chronic bronchitis).
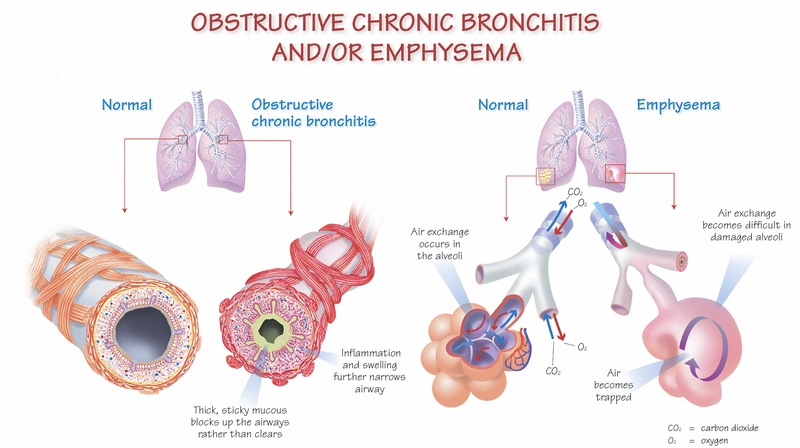
Image : Mieux vivre avec une MPOC
People with COPD often feel tired and may be short of breath doing tasks like getting out of bed, dressing, cooking, etc. They may have difficulty with their daily activities.
Treatments for chronic obstructive pulmonary disease
There is no cure for COPD, but different ways are available to ease symptoms, reduce complications and even slow the progression of the disease. For smokers, the first treatment is to stop smoking. There are also pharmacological treatments that can control the symptoms of the disease: bronchodilators, anti-inflammatories and other medicines. Oxygen therapy is also prescribed in some cases to increase the level of oxygen in the blood. Adopting a healthy lifestyle is also recommended as a treatment for the disease, including participating in regular physical activity.
Physical activity to live better with chronic obstructive pulmonary disease
The nature and severity of COPD symptoms may suggest that it is risky to be physically active, but on the contrary, it has several benefits. For people living with this condition, simple efforts of daily living are difficult due to their general lack of stamina, spontaneous shortness of breath, and loss of muscle strength. The right exercise program can improve muscle strength, increase exercise tolerance, and even reduce fatigue. It allows you to move more and move better by reducing your shortness of breath at rest and during exertion.
People with COPD may see their symptoms improve with physical activity when it is especially suited to the condition. As a result of the disease, organs such as the heart, lungs, and muscles have to work harder to produce moderate exertion. This could be improved by practicing regular physical activity. For example, stronger muscles allow you to produce more movement before you get tired. Moreover, physical activity can help maintain a healthy weight, which lowers your risk of heart disease and joint problems, in addition to strengthening your bones. Other benefits are also well known: increased energy level, improved sleep, decreased symptoms of depression, reduced pain, etc. All these benefits promote the maintenance of autonomy and reduce the risk of hospitalization as well as all the consequences of a sedentary lifestyle.
Exercises to promote when living with chronic obstructive pulmonary disease
The targets of pulmonary rehabilitation are the lungs and muscles, hence the importance of having a program that focuses on these elements, but also on cardiovascular capacity. It is important to favor exercises performed in positions where the airways are open in order to benefit from better oxygenation and better flexibility of the rib cage when performing the movements. However, the person should avoid lying positions that place additional pressure on the rib cage, making breathing activity even more difficult. When prescribing exercises, special attention should be paid to the opening of the rib cage and the flexibility of the rib cage, as a very tight breathing muscle makes the breath shorter by compressing the chest. To free the thorax and facilitate the work of the diaphragm during standing exercises, favor a position slightly tilted forward while breathing between each repetition. In fact, deep breaths are more effective for better gas exchange, so it would be relevant to breathe quietly by taking deep breaths and to exhale at length, throughout the movement.
With regard to the choice of exercises, it is important to include in the program aerobic activities, which promote the improvement of cardiovascular capacities, such as stationary cycling and walking, as well as muscle building exercises. The use of a weight system is not necessary. Strengthening can be done with small dumbbells, a rubber band, or even just your body weight. A complete program should also include flexibility exercises.
A moderate intensity is sought during the exercises, that is to say a perception of effort which is situated around 4 to 6 on a scale of 10. Cardiovascular exercises can be performed continuously for several minutes with an intensity that stay closer to 4 out of 10 or at intervals (a short period of exertion followed by a recovery period) to an intensity closer to 6 out of 10. In all cases, it is essential to ensure progress in starting with shorter exercise times and eventually increasing it to 20 to 60 minutes. It is recommended that people living with COPD exercise three times per week, but this frequency can be adjusted according to the needs and condition.
Kinesiologist’s advice for people with chronic obstructive pulmonary disease
Practice the pursed-lip breathing technique and then introduce it into workouts! This technique is well known to most people who live with COPD. This technique is very important in the practice of physical activity. It consists of taking a slow breath, ideally through your nose, then slowly exhale through your mouth, pursing your lips as if you are about to whistle. It is important to take more time for exhalation than for inhalation. When working out, it is important for a person with COPD to be alert to their symptoms and to stop if they feel dizzy, very short of breath, or if their heart is beating abnormally fast. In this case, assume a position slightly tilted forward, resting the hands on a piece of furniture or on the knees, relax the shoulders and practice pursed-lip breathing.
Resources for understanding the importance of physical activity for people living with chronic obstructive pulmonary disease
Several resources are available to better understand the effects of physical activity and encourage people to get started. Here is an example: Move to live better with my COPD – CHUM. In order to reduce the risks of side effects and promote the success of the process, monitoring by a team of health professionals, including a kinesiologist, can be very useful and recommended.
Bajac, E., Colbrant, C., & Reychler, G. (2015). Effets de l’exercice physique, et de la respiration lèvres pincées sur la ventilation pulmonaire chez les patients BPCO. Kinésithérapie, la Revue, 15(168), 20. doi:https://doi.org/10.1016/j.kine.2015.09.007
Spruit, M. A., Singh, S. J., Garvey, C., ZuWallack, R., Nici, L., Rochester, C., . . . Wouters, E. F. (2013). An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med, 188(8), e13-64. doi:10.1164/rccm.201309-1634ST






Comments